|
TPA audio player
|

Welcome to our new article, created by Plurals for Plurals. In this piece, we delve into the history of the term ‘Imitated DID‘, aiming to inform our community about the origins of this ableist term.
- Ableism, sanism, pluralphobia, shame
- Discussion on Dissociative Identity Disorder (DID)
- Mention of Satanic Panic
- Discussion on mental health diagnosis and misdiagnosis
- Mention of controversial therapies (e.g., recovered memory therapy)
- Discussion on trauma and abuse
- Discussion on borderline personality disorder
- Mention of self-diagnosis
This article explores the term ‘Imitated DID’ (Dissociative Identity Disorder), first coined by Boon and Draijer in 1999 and recently resurfaced in mental health discussions. The term emerged during a time of controversy surrounding DID, serving as a protective mechanism for the mental health field. However, it can contribute to the stigmatization of those with DID and lead to misdiagnosis and inappropriate treatment. The article critiques a 2021 study that used the term, raising ethical concerns about transparency and informed consent. It calls for a more inclusive approach to understanding DID and plurality, advocating for patient autonomy, transparency, and respect for peoples’ lived experiences.
Introduction
Recently the term imitated DID has resurfaced inside the community, after McLean used the term in their 2023 public video titled: Social media and the rise of self-diagnosed Dissociative Identity Disorder (DID) You can still sign the petition which already has over 2000 signatures by clicking here.
We say resurfaced, even though you probably have never heard of the term imitated DID before the McLean video. But it’s not a new term. It was, as far as we can find back from before the general internet, published in 1999 by Boon and Draijer, 2 Dutch DID researchers. Who mentioned they have observed imitated DID from the early 80’s. So one thing is certain, it’s not TikTok that is causing ‘this’ phenomenon.
It was brought up again in 2021 when a study from Poland was published, a study together with Boon.
And it was brought up again in 2022 in the ISSTD private conference session around the same topic as the public McLean video.
We already wrote an article on why non-disordered Plurals do not have factitious disorder and also aren’t malingering. They are Plural, for cultural, spiritual, neurodivergent, or other reasons that most do not yet understand. But there is another group of people with DID/OSDD and/or Plurality who aren’t getting the diagnosis or treatment they need. They are disproportionately likely to be from lower socioeconomic backgrounds, live in areas where trauma and dissociation informed treatment is hard to find, or belong to racial and ethnic minority groups. These are also the individuals who are often underrepresented in research about Dissociative Identity Disorder.
In 1999 Boon and Draijer wrote their explanation for the term they coined, at the start of their paper they titled Imitated DID – patient at risk, therapist at risk:
‘’Since the late 1980s the authors have been confronted with cases of imitated dissociative identity disorder (DID) in Holland. Because DSM-IV defines “factitious disorder” as intentional, the term “imitation of DID” is used here for patients who, partly unconsciously motivated, simulate a DID profile. DID can be imitated due to contagion, to iatrogenesis, or to both. The core dynamics are: (1) the avoidance of responsibility for negative behavior, found mostly in patients with a borderline or antisocial personality disorder; and (2) the compensation for an overwhelming feeling of not being seen. The last, “hysterical,” dynamic is characterized by identity disturbances varying in severity according to the underlying borderline personality structure. Four cases are described. Differentiating between genuine and imitated DID requires systematic assessment by an experienced clinician. Even then this is difficult, in particular differentiating between flamboyant genuine DID, with coexisting histrionic personality disorder (a minority of patients with genuine DID), and simulated cases. Diagnostic and treatment implications are discussed.’’
1999
In 1999 only 5 years had passed since Multiple Personality Disorder was changed to Dissociative Identity Disorder. This era also marked the ending of the many lawsuits that were brought to court during the satanic panic. An era in which large institutions lost millions in lawsuits, in member fees, and by the closures of their facilities for Multiples.
As part of the Satanic Panic, there were cases where therapists, using controversial methods like recovered memory therapy, led patients to believe they had repressed memories of traumatic experiences (including satanic ritual abuse) and multiple personalities. Some patients later came to believe that these memories and diagnoses were false, implanted by suggestive therapeutic techniques, leading to a number of high-profile lawsuits against therapists and hospitals in the 1990s.
The Wikipedia article for the ISSTD explains: ‘’After years of controversy, between 1993 and 1998, the ISSTD entered what 1999 president Peter Barach called a “crisis”. Between 1993 and 1998 the organization lost almost half its membership, about fifteen hundred people. In 1998, the society’s journal, Dissociation, ceased publication. By 1999 staff was being let go.’’
This is the landscape in which Boon and Draijer wrote their paper ‘’Imitated DID – patient at risk, therapist at risk’’ and this is why psychology wants to avoid happening again, which Imitated DID helps them do.
There is no Imitated Borderline, Imitated Depression, Imitated PTSD, Imitated [insert a DSM label here] – DID is the only disorder that has a term like Imitated DID accompanying it.
The singularity of the term “Imitated DID” in the realm of psychological disorders is not coincidental, but rather, a reflection of the unique challenges and controversies that have historically surrounded Dissociative Identity Disorder. The term emerged from a time of crisis within the mental health community, when the legitimacy of DID was under intense scrutiny and skepticism. It was an era marked by the Satanic Panic, false memory controversies, and high-profile lawsuits, all of which placed DID in the eye of a storm. As such, the term “Imitated DID” can be seen as a product of this turbulent history, a protective mechanism designed to shield the field from further controversy. Dissociative Identity Disorder (DID) stands out from other disorders due to its complex interplay of multiplicity and identity, the potential for its manifestation to be influenced externally, and its historical entanglement with legal and ethical quandaries. It is this unique environment that Boon and Draijer believed necessitated a term like ‘Imitated DID’.
How They Took the Multiple out of Multiplicity
Read the article to learn more about the history of the term Dissociative Identity Disorder.
The real risks for patients is the term Imitated DID
In the 1999 paper titled “The Imitation of Dissociative Identity Disorder: Patients at Risk, Therapists at Risk” by Nel Draijer and Suzette Boon, the authors present only four case studies to support their argument about the existence of “Imitated Dissociative Identity Disorder (DID)”. The paper discusses various risks associated with this supposed condition, including drug abuse, manipulation by older partners, a history of multiple therapists, accusations of abuse, suicidality, hospitalizations, and physical pain. However, it’s important to note that these risks are not exclusive to “Imitated DID”. They could be attributed to a variety of other mental health conditions or social issues. For instance, drug abuse and manipulation by an older partner could be associated with a range of mental health and social problems, not just imitated DID. Similarly, a history of multiple therapists and accusations of abuse could indicate a complex mental health history involving various disorders, possibly comorbid with DID/OSDD or non-disordered Plurality. Therefore, the attribution of these risks solely to “Imitated DID” may oversimplify the complex nature of mental health and potentially overlook other contributing factors or conditions.
The term “Imitated DID” not only serves to protect therapists but also poses significant risks to patients. It provides a convenient label that can be used to dismiss patients’ experiences and narratives, particularly when they do not align with the therapist’s expectations or beliefs, when patients speak up, demand personhood, or complain. This can lead to misdiagnosis, inappropriate treatment, and even harm to the patient.
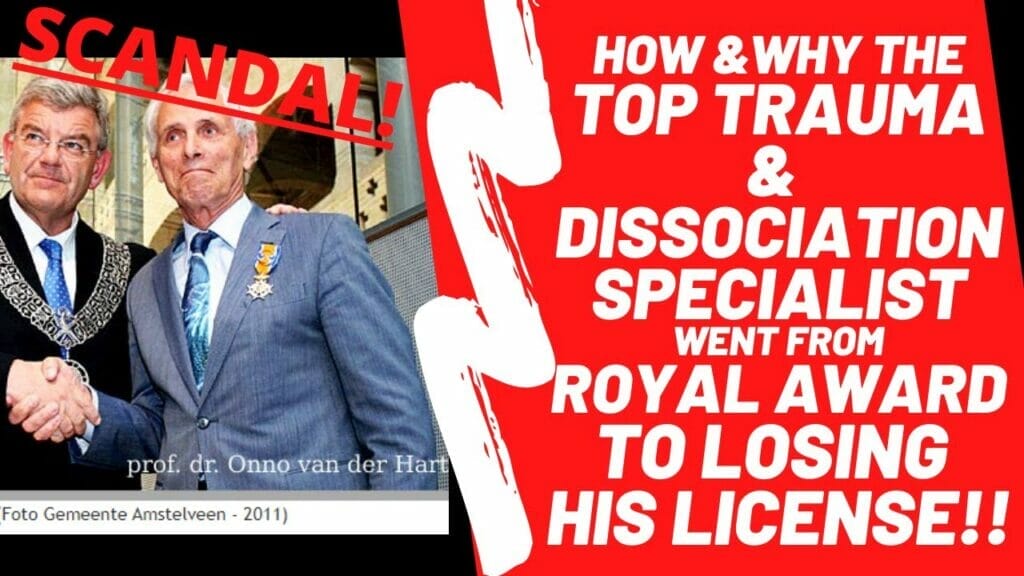
The case of Onno van der Hart, a previously prominent figure in the field of trauma and dissociation, and one of the authors of the Theory of Structural Dissociation, serves as a stark reminder of these risks. Van der Hart was stripped of his license following allegations of misconduct, including the inappropriate use of therapeutic techniques and boundary violations. His fall from grace underscores the potential for misuse of power in therapeutic relationships, particularly when dealing with complex and often misunderstood conditions like DID.
When patients are labeled with “Imitated DID”, their stories can be easily dismissed, and their experiences invalidated. This not only undermines their trust in the therapeutic process but also leaves them vulnerable to exploitation and abuse. Bad actors, like van der Hart and others who lost their licenses in the 1980s and 1990s, can misuse their power under the guise of therapy, causing significant harm to their patients.
The term “Imitated DID” thus represents a double-edged sword. While it may serve to protect therapists from controversy and legal repercussions, and maybe helps some people who do not have DID and are not Plural in other ways help understand their experiences and behavior, it also poses significant risks to patients. It’s a stark reminder of the power dynamics inherent in mental health care and the need for greater accountability, transparency, and respect for patient autonomy. Mental health professionals have a responsibility to prioritize the well-being and interests of their patients, and this includes acknowledging and validating their experiences, rather than dismissing them as “imitated”. It’s crucial that the mental health community learns from the past and takes active steps to prevent such abuses of power in the future.

2021
The 2021 Polish study in question focused on a small sample of six participants, selected from a larger pool of 86 individuals, who were part of a broader research project exploring dissociation and alterations in consciousness. The participants were not explicitly informed that they were being evaluated for both genuine and imitated Dissociative Identity Disorder (DID), which raises ethical concerns about transparency and informed consent. The study also appears to overlook the DSM-5’s recognition of self-reported signs and symptoms as valid indicators of mental health conditions like DID. Instead, the researchers relied on their own assessments and interpretations, which led them to diagnose some participants with Borderline Personality Disorder (BPD) rather than DID. This approach is here criticized for potentially dismissing the lived experiences and self-reports of the participants. Furthermore, the use of the BPD diagnosis has been controversial in some contexts, as it has been historically used to dismiss peoples’ experiences and realities, and in some cases, has been weaponized as a tool for control, silencing, and oppression. Therefore, it’s crucial to approach such studies with a critical eye, acknowledging the potential for bias and the importance of respecting individuals’ self-reported experiences.
The use of the term “Imitated DID” can inadvertently contribute to the stigmatization and marginalization of people with DID/OSDD. It can create a climate of suspicion and doubt, where people feel the need to prove the authenticity of their experiences. This is particularly concerning given the high rate of misdiagnosis associated with DID. Research shows that for most people, it takes six to twelve years while already in the mental health care system before they are correctly diagnosed with DID. In this context, the focus on “Imitated DID” can feel like a diversion from the more pressing issue of improving diagnostic accuracy and reducing the time it takes for people to receive a correct diagnosis.
Borderline Personality Disorder (BPD)
The diagnosis of Borderline Personality Disorder (BPD) within the context of the 2021 Polish study has sparked controversy. BPD is a complex condition that is often misunderstood, and it’s crucial to acknowledge that individuals with BPD have their own unique experiences and realities that deserve to be validated and understood. Historically, the diagnosis of BPD has been misused in ways that have dismissed or invalidated peoples’ experiences. However, it’s essential to recognize that this misuse is not a reflection of the people living with BPD, but rather a systemic issue within mental health care that needs to be addressed.
The participants in the Polish study, who were invited for evaluation, resided in a country where access to mental health resources, particularly for complex dissociative disorders, is limited. This scarcity of resources can make the prospect of participating in such a study particularly appealing, as it may offer a rare opportunity for people to have their experiences validated and understood.
This is particularly concerning for those participants who were ultimately diagnosed with BPD. It’s important to remember that a diagnosis of BPD is not a dismissal of an individual’s experiences, but rather a different framework for understanding their mental health. People with BPD often experience intense emotions, difficulty in relationships, and a fear of abandonment, among other symptoms. These experiences are valid and real, and they deserve to be treated with respect and understanding, and this label should never be used against someone, whether the diagnosis of BPD is accurate or not, but sadly it happens too often.
The disappointment and frustration these study participants may have felt upon receiving this diagnosis underscore the need for a more sensitive, accurate, and patient-centered approach to diagnosing and treating mental health conditions. It’s a stark reminder of the importance of cultural sensitivity and respect for peoples’ lived experiences in mental health research and practice. It also highlights the need for greater accessibility and inclusivity in mental health services, particularly in regions where such resources are scarce.
Both those with DID and BPD deserve to have their experiences validated and understood. The use of terms like “Imitated DID” can contribute to stigma and misunderstanding, and it’s crucial for the mental health community to work towards a more inclusive and respectful understanding of these complex conditions. This includes recognizing the potential for bias in diagnosis and treatment, and advocating for research and practices that respect and validate the lived experiences of all.
Theory of Structural Dissociation
However, it’s worth noting that one of the study’s authors, Boon, is also a co-author of the Theory of Structural Dissociation (ToSD), along with Kathy Steele and Onno van der Hart. They present on the theory together at conferences and have developed a skills training manual for patients with complex dissociative disorders titled “Coping with Trauma-Related Dissociation: Skills Training for Patients and Therapists”. The ToSD posits that all trauma disorders, including BPD, involve the presence of Emotional Parts (EPs) and Apparently Normal Parts (ANP). Therefore, Boon’s suggestion that those with imitated DID may have BPD could be seen as a confirmation of the ToSD. This indirect benefit to Boon and her colleagues raises further questions about potential conflicts of interest and the need for transparency in the field of DID research. It’s a reminder of the importance of critical engagement with research, particularly in areas as complex and contested as DID and plurality.
System Responsebility
System Responsibility is a key concept within the Plural community. I’m bringing this topic up, because the 1999 paper starts out by explaining that some people with Imitated DID have the avoidance of responsibility for negative behavior. Essentially, System Responsibility refers to the shared accountability of all members within a System. Just like in a team, every member has their roles, responsibilities, and contributions. In the context of Plurality, each Headmate is responsible for their actions, decisions, and their impact on the overall wellbeing of the system. It’s about understanding that each Headmate within a system, while unique with their own desires and needs, co-exists with others in the same system. The actions of one can impact others within the system, underscoring the importance of mutual respect and understanding. It’s a process of communication, understanding, and mutual respect, fostering a sense of harmony and collaboration within the system. This means that every member of the system acknowledges their actions and accepts the individual and collective consequences, whether positive or negative. Responsibility is not a skill one is born with, but it is taught by our caregivers in childhood. Many people with DID haven’t received the correct example by our caregivers, as they were our abusers and perpetrators. System responsibility is not a skill one is born with either, but rather is learned and honed over time within the system. It requires ongoing effort, communication, and mutual respect among all system members, and is often a topic worked on in the therapy of genuine DID/OSDD Systems. It’s important that clinicians meet Plurals where they are at and teach them the skills they need as a System, including System responsibility.
Shame
The use of shame as a criterion for diagnosing a mental health disorder is deeply problematic and raises significant ethical and practical concerns. At its core, this approach implies that people with genuine DID must internalize negative societal attitudes – such as pluralphobia or ableism – in order to be recognized and validated by the mental health system. This not only perpetuates harmful stereotypes and stigmas but also places an undue burden on people who are already grappling with complex mental health challenges.
Shame is a deeply personal and subjective emotion that can be influenced by a myriad of factors, including cultural norms, personal beliefs, and past experiences. It can also vary between Headmates. To use it as a diagnostic criterion risks pathologizing normal emotional responses and invalidating the diverse experiences of people with mental health conditions. Moreover, it can discourage people from seeking help, as they may fear being judged or misunderstood based on their emotional responses.
Instead of relying on shame as a diagnostic criterion, mental health professionals should strive to create an environment that fosters understanding, acceptance, and validation. This involves recognizing and challenging societal prejudices, such as pluralphobia and ableism, and advocating for a more inclusive and compassionate approach to mental health care. It’s crucial to remember that mental health disorders are not a sign of personal failure or weakness, but rather, they are complex conditions that require empathy, understanding, and appropriate care. And as Brene Brown explains, in order to empathize with someone, you must be willing to believe them as they see it, and not how you imagine their experience to be.
Plurality
A significant oversight in these studies is the lack of consideration for plurality from a spiritual, cultural, or neurodivergent perspective. Plurality, the experience of having multiple conscious identities or selves, is not inherently pathological and can be a part of diverse cultural practices, spiritual beliefs, or neurodivergent experiences. However, these studies have narrowly focused on pathological models, such as Dissociative Identity Disorder (DID) and Borderline Personality Disorder (BPD), without considering the broader spectrum of plural experiences.
For those who find solace in the DID model, the diagnosis of BPD can feel dismissive and invalidating. It overlooks the possibility that their experiences of plurality might not be disordered but rather a different way of being. The option of non-disordered plurality, which acknowledges and validates these diverse experiences, is not discussed or considered. Similarly, Other Specified Dissociative Disorder (OSDD), which is often used to diagnose people who have significant dissociative symptoms but do not meet all the criteria for DID, is also overlooked. In the 2021 paper, OSDD is only mentioned once.
This narrow focus on pathological models can limit the understanding and treatment of plurality. It can lead to misdiagnosis, inappropriate treatment, and further marginalization of people who do not fit neatly into these diagnostic categories. It underscores the need for a more inclusive and nuanced understanding of plurality, one that respects and validates the diverse experiences and perspectives of plurals, including their self/ves reporting.
Nothing About Us - Without Us
The discourse surrounding Dissociative Identity Disorder (DID) and the term “Imitated DID” underscores the urgent need for further research, education, and a shift in perspective within the mental health field. The complexities of DID and plurality necessitate a comprehensive, nuanced, and inclusive approach that goes beyond the traditional pathological models. This includes recognizing and validating the diverse experiences of those who identify as plural, whether for cultural, spiritual, or neurodivergent reasons.
The current body of research on DID is limited and often overlooks these perspectives, leading to a narrow understanding of the disorder. This not only contributes to misdiagnosis and inappropriate treatment but also perpetuates stigma and misunderstanding. Therefore, it is crucial to invest in research that aims to improve diagnostic accuracy, reduce the time it takes for people to receive a correct diagnosis, and broaden our understanding of plurality.
However, the journey towards a more inclusive and nuanced understanding of DID and plurality cannot be undertaken without the active participation of those it directly impacts. The principle of “nothing about us, without us” must be at the forefront of this endeavor. This means involving those with lived experience of DID and plurality in all aspects of research, policy-making, and treatment approaches. Their unique insights and experiences are invaluable in shaping a mental health care system that truly understands and caters to their needs.
In this context, the work of The Refractory, a think tank by The Plural Association and Katie Keech, a clinician with lived experience Plurality, is particularly noteworthy. Comprising clinicians with lived experience, The Refractory aims to transform the mental health field by bringing the Voices of those with lived experience to the forefront. Their work underscores the importance of lived experience in shaping effective, compassionate, and inclusive mental health care. This project depends on your donations, if you are able, please contribute, every dollar helps!
Furthermore, the role of therapists in diagnosing and treating DID is crucial. Therapists need to be equipped with the knowledge and skills to recognize the signs of DID/OSDD, and Plurality, understand the intricacies of the disorder, and provide appropriate and effective treatment. This includes respecting patient autonomy, practicing transparency, and maintaining an open and non-judgmental approach.
Therapist education should also focus on understanding the broader spectrum of plural experiences and acknowledging the potential for bias in diagnosis and treatment. This is particularly important in light of the controversies surrounding the diagnosis and treatment of DID, as well as the potential harm caused by terms like “Imitated DID”.
In the end, the goal should be to create a mental health care system that respects and validates the experiences of all, regardless of whether they fit neatly into existing diagnostic categories. This requires a collective effort from researchers, therapists, and the wider mental health community to challenge existing prejudices, advocate for inclusivity, and strive for a deeper understanding of DID and plurality. The journey may be complex and fraught with challenges, but the potential benefits – improved diagnosis, effective treatment, and a more compassionate understanding of plurality – make it a journey worth undertaking.
Conclusion
In conclusion, the concept of “Imitated DID” is not only a product of a turbulent period in the history of mental health but also a reflection of the ongoing challenges in understanding and treating Dissociative Identity Disorder. It is imperative that we move beyond stigmatizing labels and divisive terminology, towards an approach that respects and validates the diversity of plural experiences. The increased focus on “Imitated DID” risks distracting us from the more pressing issue: improving diagnostic accuracy, reducing misdiagnosis, and ensuring timely and appropriate care for people with DID/OSDD. As we continue to unravel the complexities of DID, it is crucial to prioritize transparency, informed consent, and the respect for self-reported experiences. Let’s strive for a more inclusive, compassionate, and nuanced understanding of DID – one that empowers Plurals, validates their diverse and unique experiences, and ultimately, leads to better mental health outcomes for all.
As always, we encourage you and your System to follow your own truth, to soul search, to find words, labels, visions, theories and communities that aren’t only within your values but also match your lived experience and/or long term goals, so that you might find belonging and don’t have to try to fit in.
Thank you for investing the time to read this article. Please, feel free to leave comments or feedback in the comment section.
‘’The Plural Association is the first and only grassroots, volunteer and peer-led nonprofit empowering Plurals. Our works, including resources like this, are only possible because of support from Plurals and our allies.
If you found this article helpful please consider making a donation.
Together we empower more Plurals!’’
Disclaimer: Thank you for reading our peer article; we hope it was empowering, informative and helpful for you and your System. There are as many Plural experiences, as there are Plurals. So not all information on this website might apply to your situation or be helpful to you; please, use caution. We’re not doctors or clinicians and our nonprofit, our work, and this website in no way provide medical advice, nor does it replace therapy or medication in other ways.
About the authors
The Stronghold System are the proud volunteer founders & CEO of The Plural Association Nonprofit. They are from the Netherlands and reside in a 30-something-year-old body, are nonbinary, parents of an amazing child & 3 cats. They got diagnosed with Dissociative Identity Disorder over 10 years ago & also self ID as Plural.
-
Strongholdhttps://powertotheplurals.com/author/stronghold/
-
Strongholdhttps://powertotheplurals.com/author/stronghold/
-
Strongholdhttps://powertotheplurals.com/author/stronghold/
-
Strongholdhttps://powertotheplurals.com/author/stronghold/
There’s an important quote I want to mention from that 1999 study.
“Because of the naive and somehow manipulative presentation of the symptoms, the possibility of imitated DID was suspected as soon as Sandra was admitted to our department. The opportunity to observe her for several months and do extensive diagnostic assessment confirmed this impression.”
This is called confirmation bias, and is a HUGE red flag. They decided her DID was likely fake before they even started their assessment.